Vitamin D

Vitamin D is a group of fat-soluble pro hormones, the two major forms of which are vitamin D2 (or ergocalciferol) and vitamin D3 (or cholecalciferol). The term vitamin D also refers to metabolites and other analogues of these substances. Vitamin D3 is produced in skin exposed to sunlight, specifically ultraviolet B radiation.
Vitamin D deficiency can result from inadequate intake coupled with inadequate sunlight exposure, disorders that limit its absorption, conditions that impair conversion of vitamin D into active metabolites, such as liver or kidney disorders, or, rarely, by a number of hereditary disorders. Deficiency results in impaired bone mineralisation, and leads to bone softening diseases, rickets in children and osteomalacia in adults, and possibly contributes to osteoporosis. However, sunlight exposure, to avoid deficiency, carries other risks, including skin cancer; this risk is avoided with dietary absorption, either through diet or as a dietary supplement.
Sources of vitamin D in food
Very few foods are naturally rich in vitamin D, so much vitamin D intake in the industrialised world is from fortified products including milk, soy milk and breakfast cereals or supplements. Natural sources of vitamin D include:
- Fish liver oils, such as cod liver oil, 1 tablespoon. (15 mL) provides 1,360 IU (one IU equals 25 ng)
- One whole egg, provides 20 IU
- Beef liver, cooked, 3.5 ounces, provides 15 IU
The figures below are from Health Canada and are similar to the RDA for most countries. The figures basically represent the Tolerable Upper Intake Level.
The Tolerable Upper Intake Level is defined as "the highest average daily intake of a nutrient that is likely to pose no risk of adverse health effects for nearly all persons in the general population.
The recommended dietary allowances (RDA) for vitamin D are:
| Age group | RDA | Tolerable Upper Intake |
|---|---|---|
| Infants 0–6 months | 400 IU* | 1000 IU |
| Infants 7–12 months | 400 IU* | 1500 IU |
| Children 1–3 years | 600 IU | 2500 IU |
| Children 4–8 years | 600 IU | 3000 IU |
| Children and Adults 9–70 years | 600 IU | 4000 IU |
| Adults > 70 years | 800 IU | 4000 IU |
| Pregnancy & Lactation | 600 IU | 4000 IU |
Note*: Adequate Intake rather than Recommended Dietary Allowance.
Health effects of supplements
The effects of vitamin D supplementation on health are uncertain. A United States Institute of Medicine, (IOM) report states: "Outcomes related to cancer, cardiovascular disease and hypertension, diabetes and metabolic syndrome, falls and physical performance, immune functioning and autoimmune disorders, infections, neuropsychological functioning, and preeclampsia could not be linked reliably with calcium or vitamin D intake and were often conflicting." Some researchers claim the IOM was too definitive in its recommendations and made a mathematical mistake when calculating the blood level of vitamin D associated with bone health. Members of the IOM panel maintain that they used a "standard procedure for dietary recommendations" and that the report is solidly based on the data. Research on vitamin D supplements, including large scale clinical trials, is continuing.
Mortality
Low blood levels of vitamin D are associated with increased mortality, and giving supplementary vitamin D3 to elderly women in institutional care seems to decrease the risk of death. Vitamin D2, alfacalcidol, and calcitriol do not appear to be effective. However, both an excess and a deficiency in vitamin D appear to cause abnormal functioning and premature aging. The relationship between serum calcidiol level and all-cause mortality is U-shaped, Harm from vitamin D appears to occur at a lower vitamin D level in the black population than in the white population.
Bone health
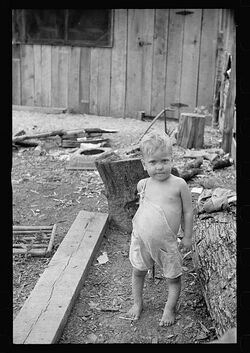
Vitamin D deficiency causes osteomalacia (called rickets when it occurs in children). Beyond that, low serum vitamin D levels have been associated with falls, and low bone mineral density.
In 2012, the U.S. Preventive Services Task Force issued a draft statement recommending that there is not enough evidence to indicate that healthy postmenopausal women should use supplemental doses of calcium or vitamin D to prevent fractures. Some studies have shown that supplementation with vitamin D and calcium may improve bone mineral density slightly, as well as decreasing the risk of falls and fractures in certain groups of people, specifically those older than 65 years. This appears to apply more to people in institutions than those living independently. The quality of the evidence is, however, poor. And there does not appear to be a benefit to bone health from vitamin D without sufficient calcium.
Cardiovascular disease
Evidence for health effects from vitamin D supplementation for cardiovascular health is poor. Moderate to high doses may reduce cardiovascular disease risk but are of questionable clinical significance.
Multiple sclerosis
Low levels of vitamin D are associated with multiple sclerosis. Supplementation with vitamin D may have a protective effect but there are uncertainties and unanswered questions. "The reasons why vitamin D deficiency is thought to be a risk factor for MS are as follows: (1) MS frequency increases with increasing latitude, which is strongly inversely correlated with duration and intensity of UVB from sunlight and vitamin D concentrations; (2) prevalence of MS is lower than expected at high latitudes in populations with high consumption of vitamin-D-rich fatty fish; and (3) MS risk seems to decrease with migration from high to low latitudes." A clinical trial sponsored by Charite University in Berlin, Germany was begun in 2011, with the goal of examining the efficacy, safety and tolerability of vitamin D3 in the treatment of Multiple Sclerosis.
Cancer
Low vitamin D levels are associated with some cancers and with worse outcomes in other cancers, but taking supplements does not appear to help people with prostate cancer. Currently evidence is insufficient to support supplementation in those with cancer. Results for a protective or harmful effect of vitamin D supplementation in other types of cancer are inconclusive.
Pregnancy
Pregnant women who take an adequate amount of vitamin D during gestation, may experience positive immune effects. Pregnant women throughout the world do not take the recommended dose of vitamin D, which could negatively impact the health of the mother and her foetus.
Acute migraines related to onset of menopause
On a personal note, a good friend of mine had been suffering acute migraines for 5 years following the start of her menopause. They were debilitating and seriously affected her life-style. She saw various doctors about this condition and even tried H.R.T. (hormone replacement therapy) - which was infective and also affected her emotionally. Finally another doctor took blood tests and noted a vitamin D deficiency. She was prescribed an 8 week course of calcium and vitamin D. Following that she has had 3 migraines in 5 months, compared to two a week before the treatment.
Other
Vitamin D appears to have effects on immune function. It has been postulated to play a role in influenza with lack of vitamin D synthesis during the winter as one explanation for high rates of influenza infection during the winter. For viral infections, other implicated factors include low relative humidities produced by indoor heating and cold temperatures that favour virus spread. Low levels of vitamin D appear to be a risk factor for tuberculosis, and historically it was used as a treatment. As of 2011, it is being investigated in controlled clinical trials. Vitamin D may also play a role in HIV. Although there are tentative data linking low levels of vitamin D to asthma, there is inconclusive evidence to support a beneficial effect from supplementation. Accordingly, supplementation is not currently recommended for treatment or prevention of asthma. Also, preliminary data is inconclusive for supplemental vitamin D in promotion of human hair growth.
Deficiency
A diet deficient in vitamin D causes osteomalacia (called rickets when it occurs in children), which is a softening of the bones. In the developed world, this is a rare disease. Low blood calcidiol (25-hydroxy-vitamin D) can result from avoiding the sun. Deficiency results in impaired bone mineralization and leads to bone-softening diseases including: Rickets, a childhood disease characterised by impeded growth and deformity of the long bones, can be caused by calcium or phosphorus deficiency as well as a lack of vitamin D; today it is largely found in low-income countries in Africa, Asia or the Middle East and in those with genetic disorders such as pseudovitamin D deficiency rickets. Rickets was first described in 1650 by Francis Glisson who said it had first appeared about 30 years previously in the counties of Dorset and Somerset. In 1857, John Snow suggested that rickets, then widespread in Britain, was being caused by the adulteration of bakers' bread with alum. The role of diet in the development of rickets was determined by Edward Mellanby between 1918–1920. Nutritional rickets exists in countries with intense year round sunlight such as Nigeria and can occur without vitamin D deficiency. Although rickets and osteomalacia are now rare in Britain, there have been outbreaks in some immigrant communities in which osteomalacia sufferers included women with seemingly adequate daylight outdoor exposure wearing Western clothing. Having darker skin and reduced exposure to sunshine did not produce rickets unless the diet deviated from a Western omnivore pattern characterised by high intakes of meat, fish and eggs, and low intakes of high-extraction cereals. The dietary risk factors for rickets include abstaining from animal foods. Vitamin D deficiency remains the main cause of rickets among young infants in most countries, because breast milk is low in vitamin D and social customs and climatic conditions can prevent adequate UVB exposure. In sunny countries such as Nigeria, South Africa, and Bangladesh, where the disease occurs among older toddlers and children, it has been attributed to low dietary calcium intakes, which are characteristic of cereal-based diets with limited access to dairy products. Rickets was formerly a major public health problem among the US population; in Denver where ultraviolet rays are approximately 20% stronger than at sea level on the same latitude, almost two thirds of 500 children had mild rickets in the late 1920s. An increase in the proportion of animal protein in the 20th century American diet coupled with increased consumption of milk fortified with relatively small quantities of vitamin D coincided with a dramatic decline in the number of rickets cases.
Osteomalacia, a bone-thinning disorder that occurs exclusively in adults, is characterised by proximal muscle weakness and bone fragility. The effects of osteomalacia are thought to contribute to chronic musculoskeletal pain, There is no persuasive evidence of lower vitamin D levels in chronic pain sufferers.
The Director General of Research and Development and Chief Scientific Adviser for the UK Department of Health and NHS said that children aged six months to five years should be given vitamin D supplements, particularly during the winter. However, vitamin D supplements are not recommended for people who get enough vitamin D from their diets and from sunlight.
Some research shows that dark-skinned people living in temperate climates have lower vitamin D levels. It has been suggested that dark-skinned people are less efficient at making vitamin D because melanin in the skin hinders vitamin D synthesis; however, a recent study has found novel evidence that low vitamin D levels among Africans may be due to other reasons. Recent evidence implicates parathyroid hormone in adverse cardiovascular outcomes. Black women have an increase in serum PTH at a lower 25(OH)D level than white women. A large scale association study of the genetic determinants of vitamin D insufficiency in Caucasians found no links to pigmentation.
On the other hand, the uniform occurrence of low serum 25(OH)D in Indians living in India and Chinese in China, does not support the hypothesis that the low levels seen in the more pigmented are due to lack of synthesis from the sun at higher latitudes. The leader of the study has urged dark-skinned immigrants to take vitamin D supplements nonetheless, saying, "I see no risk, no downside, there's only a potential benefit."
Toxicity
In healthy adults, sustained intake of more than 1250 micrograms/day (50,000 IU) can produce overt toxicity after several months; those with certain medical conditions such as primary hyperparathyroidism are far more sensitive to vitamin D and develop hypercalcemia in response to any increase in vitamin D nutrition, while maternal hypercalcemia during pregnancy may increase fetal sensitivity to effects of vitamin D and lead to a syndrome of mental retardation and facial deformities. Pregnant or breastfeeding women should consult a doctor before taking a vitamin D supplement. For infants (birth to 12 months), the tolerable upper limit (maximum amount that can be tolerated without harm) is set at 25 micrograms/day (1000 IU). One thousand micrograms (40,000 IU) per day in infants has produced toxicity within one month. After being commissioned by the Canadian and American governments, the Institute of Medicine (IOM) as of 30 November 2010, has increased the tolerable upper limit (UL) to 2500 IU per day for ages 1–3 years, 3000 IU per day for ages 4–8 years and 4000 IU per day for ages 9–71+ years (including pregnant or lactating women). Vitamin D overdose causes hypercalcemia, and the main symptoms of vitamin D overdose are those of hypercalcemia: anorexia, nausea, and vomiting can occur, frequently followed by polyuria, polydipsia, weakness, insomnia, nervousness, pruritus, and, ultimately, renal failure. Proteinuria, urinary casts, azotemia, and metastatic calcification (especially in the kidneys) may develop. Vitamin D toxicity is treated by discontinuing vitamin D supplementation and restricting calcium intake. Kidney damage may be irreversible. Exposure to sunlight for extended periods of time does not normally cause vitamin D toxicity. Within about 20 minutes of ultraviolet exposure in light-skinned individuals (3–6 times longer for pigmented skin), the concentrations of vitamin D precursors produced in the skin reach an equilibrium, and any further vitamin D that is produced is degraded.
Published cases of toxicity involving hypercalcemia in which the vitamin D dose and the 25-hydroxy-vitamin D levels are known all involve an intake of =40,000 IU (1000 µg) per day. Recommending supplementation, when those supposedly in need of it are labeled healthy, has proved contentious, and doubt exists concerning long term effects of attaining and maintaining high serum 25(OH)D by supplementation.
Source
- Information distilled from Wikipedia vitamin D article
See also
- BBC News: Cheap vitamin D 'would boost health'
- Vitamin A
- Vitamin B
- Vitamin C
- Vitamin D
- Vitamin E
- Vitamin K
- Folic acid
Find recipes that contain 'Vitamin D'
#vitamind #bones #liver #mackerel #tuna #beef #egg #cod #fish #vitamins #catfish